CHPN Test Guide
Certified hospice and palliative care nurses are leaders in the evolution of healthcare in the United States. Consumers are becoming more involved in their own healthcare decisions. They are making increasingly informed choices about what diagnostic evaluations they will submit to, and what treatment options they will accept.
Hospice and palliative care professionals lead the advocacy movement for an alternative to aggressive care for those who could benefit. Professionals in this specialty field provide support for patients and families who want a voice in the quality of life they experience during life-limiting illnesses and at end of life.
The hospice and palliative care nurse is a key component of providing such care. Certification in this specialty acknowledges the skill and expertise with which such nurses do so.
What does a certified hospice and palliative care nurse (CHPN) do?
According to the CHPN Candidate Handbook, “Hospice and palliative care is the provision of care for the patient with serious illness and their family with the emphasis on their physical, psychosocial, emotional and spiritual needs." This is accomplished in collaboration with an interdisciplinary team in a variety of settings which provide 24-hour nursing availability, pain and symptom management, and family support. Such care is delivered in any setting which is defined as the patient’s home.
CHPNs function in a variety of roles. If not providing direct patient care, they may serve as team managers, administrators, and educators, since such roles are often filled by nurses who were previously clinicians in the field.
Always, they operate within an interdisciplinary team made up of nurses, social workers, nursing assistants, chaplains, volunteers, and the medical director. All members function as a unit to collaborate and provide comprehensive care to both the patient and the family, who are also considered part of the interdisciplinary team.
Within any of these roles, CHPNs are models of professionalism and excellence. Therefore, they often serve as mentors and trainers for others. Since community health professionals often rely on the expertise of hospice and palliative care personnel to coordinate symptom relief for their patients, CHPNs frequently act in consulting roles, offering recommendations based on a common and accepted knowledge base.
Why become certified?
When nurses are able to identify themselves as CHPNs, many parties benefit. The patient and family can rest assured, knowing that they are receiving optimum care from an expert in this field. The hospice can validate that their nurses are operating from a standardized knowledge base. Peers appreciate practicing with expert colleagues. And the CHPN takes pride in knowing that she is providing excellence in care within the current standard of practice.
Preparation for the exam involves commitment; time, effort, and money. Although some employers may strongly recommend certification, this is a voluntary process. Various incentives may be offered by hospice organizations, but often, there is no financial reimbursement or monetary compensation.
Hospice nurses work in this field because they have a passion for it. Certification proves that they can provide comprehensive care to patients and families at the highest levels of excellence.
Who administers the exam?
The exam for certification in hospice and palliative care nursing is administered by the National Board for Certification of Hospice and Palliative Nurses (NBCHPN). Formed in 1993 to develop a certification program for the practice of hospice and palliative nursing, its first Certification Exam for Hospice Nurses was administered in 1994. There are over 13,000 individuals certified by this organization.
Initially credentialed as certified registered hospice nurses (CRNH), this designation was discontinued in 2002, after the 1999 credentialing change to certified hospice and palliative care nurse (CHPN).
In addition to the CHPN, the NBHPCN offers credentialing in five other hospice and palliative care specialties:
- Advanced Certified Hospice and Palliative Nurse (ACHPN®)
- Certified Hospice and Palliative Pediatric Nurse (CHPPN®)
- Certified Hospice and Palliative Licensed Nurse (CHPLN®)
- Certified Hospice and Palliative Nursing Assistant (CHPNA®)
- Certified Hospice and Palliative Care Administrator (CHPCA®)
Each certification has a four year validation period.
Eligibility
Eligibility for the exam requires that the applicant hold a current, unencumbered registered nurse license in the United States, its territories, or the equivalent of Canada and have hospice and palliatiave care experience of 500 hours in the past year or 1,000 hours in the past two years. For a complete listing of eligibility criteria, please see the CHPN Handbook.
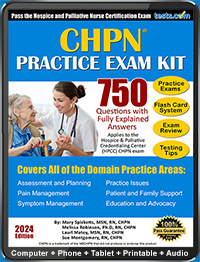
CHPN Exam Content
CHPN exam content has been developed from role delineation studies which have been obtained through a validated job analysis which reflects current practice for both hospice and non-hospice palliative settings across the country.
The CHPN exam consists of 150 questions across 5 domains of practice in caring for the adult patient and family:
- Patient Care: Assessment and Planning
- Patient Care: Pain Management
- Patient Care: Symptom Management
- Support, Education and Advocacy
- Practice Issues
Participants are given 3 hours for completion of the test. Test questions are in a computerized, multiple-choice format, containing a mix of scenario-based questions with direct content questions. Only 135 of the 150 questions are scored.
The pain and symptom management sections contain questions about medications for specific symptoms, dosages, and titration calculations, including equianalgesic dosing. All medications are referred to using generic names, with a few exceptions possible.
In summary, certification in hospice and palliative nursing is about professionalism and personal pride. It’s about providing optimal support for the patients and families such nurses care for, and care about. Certification provides assurance to patients, families, employers and colleagues that they are working with someone who operates at the highest levels of expertise, integrity and professionalism.
Want additional help preparing for the CEN? Check out our CHPN Directory to find helpful study aids.